The public health authorities in both the United States and Europe took up fundamental measures to control epidemics that dated back to Medieval times of the Bubonic Plague. They aimed to reduce the transmission of the pathogen by preventing contact. They framed their public health orders in scientific ideas of their understanding of how the influenza microbe spread through the air by coughing and sneezing, and their conception of the pathogenesis of influenza. Since they concluded that the pathogen was transmitted through the air, efforts to control contagion were organized to prevent those infected from sharing the same air as the uninfected. Public gatherings and the coming together of people in close quarters was seen as a potential agency for the transmission of the disease. The public health authorities believed that good ventilation and fresh air were "the best of all general measures for prevention, and this implies the avoidance of crowded meetings," (BMJ, 10/19/1918). This translated into the controversial and imperative measure of closing of many public institutions and banning of public gatherings during the time of an epidemic.

The rigidity of these regulations varied immensely with the power of the local health departments and severity of the influenza outbreak. In the United States, the Committee of the American Public Health Association ( APHA) issued measures in a report to limit large gatherings. The committee held that any type of gathering of people, with the mixing of bodies and sharing of breath in crowded rooms, was dangerous. Nonessential meetings were to be prohibited. They determined that saloons, dance halls, and cinemas should be closed and public funerals should be prohibited since they were unnecessary assemblies. Churches were allowed to remain open, but the committee believed that only the minimum services should be conducted and the intimacy reduced. Street cars were thought to be a special menace to society with poor ventilation, crowding and uncleanliness. The committee encouraged the staggering of opening and closing hours in stores and factories to prevent overcrowding and for people to walk to work when possible (JAMA, 12/21/1918). Some of the regulations in Britain were milder, such as limiting music hall performances to less than three consecutive hours and allowing a half-hour for ventilation between shows (BMJ, 11/30/1918). In Switzerland, theaters, cinemas, concerts and shooting matches were all suspended when the epidemic struck, which led to a state of panic (BMJ, 10/19/1918). This variation in response was most likely due to differences in authority of the public health agencies and societal acceptance of their measures as necessary. This necessitated a shared belief in the concept of contagion and some faith in the actions of science to allow them to overcome this plague.
The most frequently discussed and debated public health measure in the journals of the period was the closure of the schools. In Britain the prevalence of the epidemic led to the closure of the public elementary schools (BMJ, 11/30/1918). In France, students with any symptoms and their siblings were to be excluded from school. If three fourths of the students were absent then the whole class was to be dismissed for 15 days (JAMA, 12/7/1918). Some believed closing schools to be a useful measure to control infection but complained that it often occurred too late, after most students and teachers were sick (BMJ, 10/19/1918). In the United States, school closure was not as widely accepted. One article in JAMA said that, "the desirability of closing schools in a large city in the presence of an epidemic is a measure of doubtful value," (10/5/1918). The APHA Committee debated its value too, questioning the effectiveness against the loss of educational standards. Generally, school closure was thought to be less effective in large urban metropolises than in rural centers where the school represented the point of dissemination of the infectious agent. The closing of schools and other public institutions as public health regulations to reduce the epidemic was not universally accepted. One editorial in the BMJ states that "every town-dweller who is susceptible must sooner or later contract influenza whatever the public health authorities may do; and that the more schools and public meetings are banned and the general life of the community dislocated the greater will be the unemployment and depression," (12/21/1918).
The more restrictive methods of infection control issued by public health departments were quarantines and the isolation of the ill. These measures required a sacrifice of individual liberty for the societal good and therefore required a strong public health authority. Both the Illinois and New York State Health Departments ordered that patients must be quarantined until all clinical manifestations of the illness subsided. They held that the danger of the influenza epidemic was so grave that it was imperative to secure isolation for the patient (JAMA, 10/12/1918). The members of the APHA committee agreed in their report, saying that patients with influenza should to be kept in isolation. Because of the strain on facilities, only severe cases were to be hospitalized while mild influenza patients were to remain at home. The APHA also supported institutional quarantines to protect people from the outside world in establishments like asylums and colleges (JAMA, 12/21/1918). The use of institutional quarantines was applied to the many military training camps set up in the United States to prepare soldiers for war. These camps, with masses of men from throughout the country, were prime targets of huge influenza epidemics. The men were kept in strict isolation once ill and entire camps was often quarantined (JAMA, 4/12/1919). These measures were easily implemented in these camps where men were already committed to their country and the authority of the government.
The Committee of the American Public Health Association (APHA) issued a report outlining appropriate ways to prevent the spread and reduce the severity of the epidemic. They noted first that the disease was extremely communicable and "spread solely by discharges from the nose and throats of infected persons." They sought to prevent infection by breaking the channels of communication such as droplet infection by sputum control. They believed that infection occurred by the contamination of the hands and common eating and drinking utensils. Thus they called for legislation to prevent the use of common cups and to regulate coughing and sneezing. They wanted to initiate education programs and publicity on respiratory hygiene about the dangers of coughing, sneezing and the careless disposal of nasal discharges. They aimed to teach people the value of hand-washing before eating and the advantages of general hygiene (JAMA, 12/21/1918). Public Health Departments issued Flu Posters to educate the community and reduce the spread of infection. The members also noted that the response should vary according to the type of community and the living conditions. Measures were to be adapted to rural or metropolitan areas, with a centralized coordination to enforce compulsory reporting and canvassing for cases.
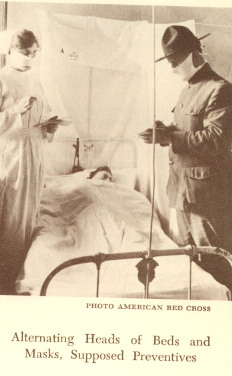
Public Health agencies applied the principles of contagion to methods of hygiene and a regard for ventilation in their suggestions for reducing the spread of the illness and preventing disease. They held that well ventilated, airy rooms promoted well-being, (BMJ, 11/16/1918). Preventative measures built upon the same ideas of transmission and the germ theory of disease. These ideas were practiced in the hospitals as special influenza wards for influenza patients were created and the number of beds per ward was decreased to reduce the transmission of the disease. Those with complications such as pneumonia were separated from the rest to prevent the others from progressing to this more fatal state (BMJ, 11/2/1918). Sheets were hung between the beds to mimic isolation in limited closed quarters to provide a cubicle for each patient. No patient was allowed to leave their bed until they were fever free for 48 hours. In the military camps, soldiers were instructed to eat 5 feet apart in the mess halls. Head to foot sleeping was also implemented to reduce the sharing of air space (JAMA, 4/12/1919). One camp used these ideas of prevention via ventilation and boasted of their results. They claimed their rampant influenza epidemic terminated once men were kept out in the open with sunlight or in open, airy halls and prevented from gathering (JAMA, 12/14/1918).
One of the key aspects of prevention was the use of disinfection and sterilization methods. The practical prevention guidelines utilized the recent developments made by Lister and others of the necessity antiseptic conditions. All bedding and rooms were to be periodically disinfected to kill whatever pathogen pervaded them. In naval ambulance trains this was executed by washing down the train with a weak izal antiseptic solution (BMJ, 11/23/1918). The produced sputum, thought to be riddled with the microbe, was to be destroyed. In one hospital the sputum cups were emptied and disinfected twice daily, while nasal discharges were collected in paper napkins. An antiseptic hand solution was placed conveniently for those on duty in the influenza ward (JAMA, 4/12/1919). One French report also suggested that the staff of influenza wards should wear blouses inside the ward and remove them when leaving (BMJ, 11/2/1918). These disinfection procedures of prevention utilized scientific ideas of germ theory to reduce transmission.
The gauze mask was another prevention method using similar ideas of contagion and germ theory. In the United States it was widely accepted for use in hospitals among health care workers. The face masks consisted of a half yard of gauze, folded like a triangular bandage covering the mouth, nose and chin (BMJ, 11/2/19118). These gauze masks acted to prevent the infectious droplets from being expelled by the mouth and from the hands, contaminated with microbe from being put to the mouth. The barrier from the hands was thought to be more important than the barrier from the air. The mask was also worn in some regions by the general population. In San Francisco the gauze masks were made a requirement of the entire population in a trial ordinance. This was later expanded to include San Diego in December. This rhyme was a popular way to remind people of the ordinance.

The members of the APHA committee also suggested ways to increase the natural resistance to the illness. They stated that nervous and physical exhaustion should be avoided. People were encouraged to maintain proper rest, to get fresh air and maintain general hygiene. The French report also encouraged avoiding over-fatigue and exposure to the cold (BMJ, 11/2/1918). The Royal College of Physicians shared this opinion saying that the chilling of the body should be prevented by wearing warm clothing out of doors. They also claimed that good nourishment of food and drink was desirable, saying that chill and over-exertion...have evil consequences," (BMJ, 11/16/1918). These methodologies unlike the preventative measures do not appear to have a strong scientific basis. Rather, they reflect common societal ideas about the wellness and the ability to fight infection. Thus to a degree, the medical and public health officials were still using common sense notions to combat this new infectious terror.

One method of preventing infection, however was more scientific, more elaborate and more controversial. This was the gargling and rinsing out of the nasopharynx with antiseptic solution. Physicians held that since the disease was transmitted through the upper respiratory passages, it made sense to disinfected the nose and mouth to prevent infection. One method was to gargle with warm water mixed with chlorinated soda. A Dr. F. W. Alexander recommended electrolytic disinfection fluid as mouth wash for influenza to be gargled and sniffed up the nose (BMJ, 11/2/1918). Others gargled and sprayed the nasopharynx with a weak solution of carbolic acid and combined it with quinine to prevent infection (BMJ, 11/23/1918). A more serious method of cleansing and disinfecting the nasal spaces and upper air passages was suggested by Dr. James Bach. He advocated a powder of boric acid and sodium bicarbonate. The powder was to be blown into the nose which would then dissolve and by osmotic pressure induce mucus flow to wash the membranes (JAMA, 12/7/1918). This method has a scientific basis but little scientific proof of efficacy. They worked as well as some of the treatments invented to cure influenza which were based on scientific ideas but not scientific results. The APHA members believed that gargling had no value as they cleared out the protective mucus barrier to infection.
The American Public Health Association committee members believed that the best way to prevent infection was through the use of vaccines. Vaccines could prevent or mitigate infection with influenza and the frequently fatal complications of the illness due to the influenza bacillus or strains of streptococci and pneumonococci. They believed that the current vaccines under development should be tested and administered if useful to prevent infection. The committee suggested the use of the experimental vaccines on susceptibles with equal subjects and controls and under proper scientific methodology. However, they acknowledged that the cause of the influenza was unknown and therefore an effective vaccine had no "scientific basis," (JAMA, 12/21/1918). These public health officials shared the perceptions of the scientific and medical community of the influenzal disease and its origins.
 Back to the Top of the page.
Back to the Top of the page.
 To the main
Influenza Pandemic page.
To the main
Influenza Pandemic page.
 To the
Science and Medicine page.
To the
Science and Medicine page.